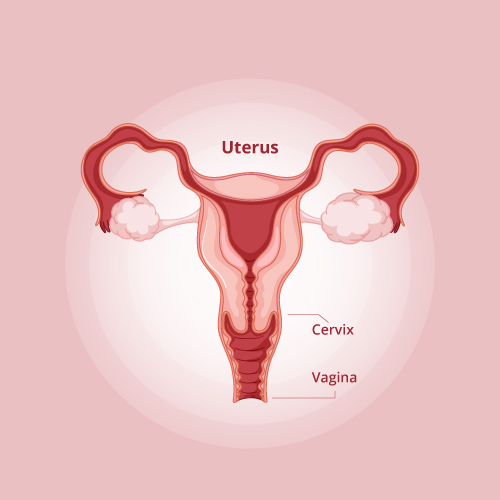
What is Cervical cancer
Cervical cancer begins in the cells of the cervix - the lower part of the uterus that connects to the vagina. Various strains of the Human Papilloma Virus (HPV), a sexually transmitted infection, play a major role in causing cervical cancer. When exposed to HPV, a woman's immune system typically prevents the virus from doing harm. In a small group of women, however, the virus survives for years, contributing to the process that causes some cells on the surface of the cervix to become cancer cells.
Incidence & Epidemiology
- More women in India die from cervical cancer than in any other country.
- The incidence of cervical cancer is higher in rural areas as compared to cities
- Around 1.23 lakh new women are diagnosed with cervical cancer in India and 67,500 women die of it every year

Vaginal bleeding after intercourse, between periods or after menopause

Watery, bloody vaginal discharge that may be heavy and have a foul odor

Pelvic pain or pain during intercourse
Main types of Cervical Cancer

Squamous cell carcinoma
This type of cervical cancer begins in the thin, flat cells (squamous cells) lining the outer part of the cervix, which projects into the vagina. Most cervical cancers are Squamous cell carcinomas.

Adenocarcinomas
This type of cervical cancer begins in the column-shaped glandular cells that line the cervical canal.
Risk Factors
Diagnosis and Screening
Screening for Cervical Cancer
Diagnosis for Cervical Cancer
Imaging Tests help to determine whether cancer has spread beyond cervix:
-
1Cancer confined to the cervix
-
2Cancer reached upper portion of vagina
-
3Cancer spread to lower portion of vagina
-
4Cancer spread to nearby organs
Significance of HPV vaccination
-
Protection is seen only when the vaccine is given before infection with HPV.
-
Vaccine should preferably be introduced to parents as a cervical cancer-preventing vaccine and not as a vaccine against a sexually transmitted infection.
-
Vaccines are not 100% protective against cervical cancer and not a replacement for periodic screening. Hence, screening programs should continue as per recommendations.
-
Gardasil marketed by Merck (quadrivalent vaccine)
-
Cervarix marketed by Glaxo Smith Kline (bivalent vaccine)
Guidelines for testing and screening
-
All women should begin cervical cancer screening when they are 21 years old. Screening should be done every 3 years in women with no history of abnormal Paps. More frequent screening may be needed if any abnormal cells are found or if HPV is present.
-
Beginning at age 30, women who have had 3 normal Pap test results in a row should be screened every 5 years with both a Pap smear test AND a screening test for - high risk type - HPV infection. Another acceptable option is to be screened every 3 years with only the Pap test. Women who have certain risk factors such as diethylstilbestrol (DES) exposure before birth, HIV infection, or a weakened immune system due to organ transplant, chemotherapy, or chronic steroid use should continue to be screened annually.
-
Women 65-70 years of age or older who have had 3 or more normal Pap tests in a row and no abnormal Pap test results in the last 20 years should stop having cervical cancer screening. Women with a history of cervical cancer, DES exposure before birth, HIV infection or a weakened immune system should continue to have screening as long as they are in good health.
-
Women who have had a total hysterectomy (removal of the uterus and cervix) should also stop having cervical cancer screening, unless they have a history of cervical cancer or precancer. Women who have had a hysterectomy without removal of the cervix should continue to follow the guidelines above.
HPV strains categorization
-
Over 118 serotypes of HPV have been discovered, of which 15-20 are oncogenic.
-
On the basis of association with cervical cancer, genital HPVs are further grouped into:
-
High-risk types
-
Probable high-risk types
-
Low-risk types
-
-
In India as well as globally, high-risk type HPV-16 and 18 contribute over 70% of all cervical cancer cases (the most prevalent being HPV-16 in at least 50-60% and HPV-18 in at least 10-12%).
-
Non-oncogenic HPV serotypes-6 and 11 contribute over 90% of benign genital infections such as genital warts..
-
Oncogenic HPV serotypes have also been implicated in the causation of anal, vulvar, vaginal, penile and oropharyngeal cancers.
Importance of genotyping Genotypes covered in our test
Persistent infection with oncogenic types of HPV followed by HPV DNA integration into the cellular genome is a required precursor in the pathway leading to cervical neoplasia in females.
Routine screening for HPV DNA in females reduces the incidence of cervical cancer and in males is linked to OSCC.
We do the qualitative detection & genotyping of 12 high risk genotypes known to be associated with cervical cancer & 2 low risk genotypes of HPV which are linked to genital warts.
-
High risk HPV genotypes: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58 & 59
-
Low risk HPV genotypes: 6 & 11
















